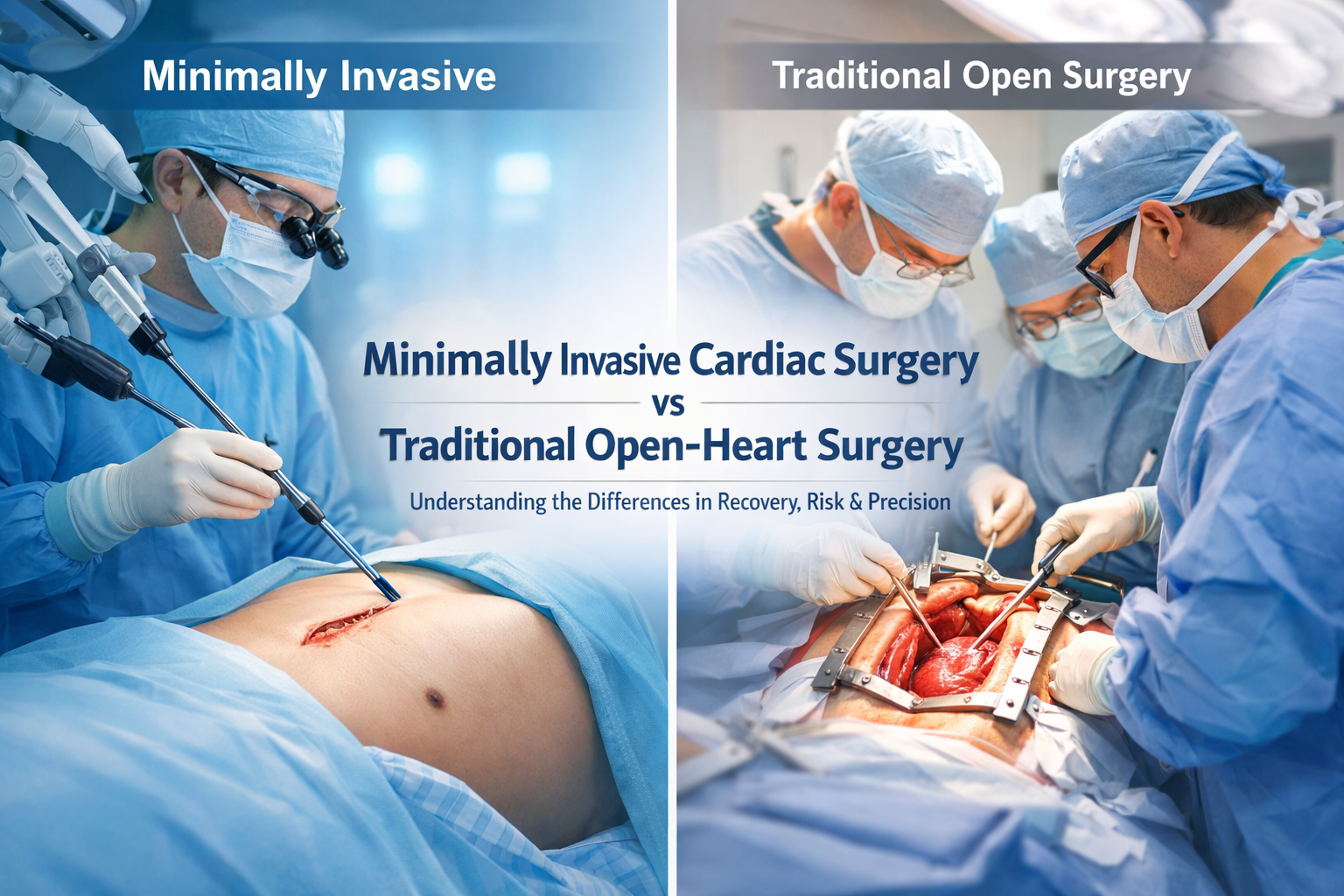
What Patients Need to Know Before Choosing the Right Approach
Heart surgery has evolved dramatically over the past few decades. What once required large incisions, prolonged hospital stays, and months of recovery can now, in selected cases, be performed through smaller incisions with faster healing and less discomfort.
If you or a loved one has been advised to undergo heart surgery — whether for blocked arteries, valve disease, or advanced heart failure — you may hear two terms:
- Traditional Open-Heart Surgery
- Minimally Invasive Cardiac Surgery (MICS)
Understanding the differences between these approaches can help you make an informed decision in consultation with your cardiac surgeon.
What Is Traditional Open-Heart Surgery?
Traditional open-heart surgery involves:
- A long vertical incision in the center of the chest
- Splitting the breastbone (sternotomy)
- Use of a heart-lung machine (cardiopulmonary bypass) in most cases
- Direct access to the heart
This approach has been the gold standard for decades and remains highly effective for complex procedures.
Common Surgeries Performed via Traditional Open-Heart Approach
- Coronary Artery Bypass Grafting (CABG)
- Valve repair and replacement
- Aortic surgery
- Heart transplant
- Complex congenital heart surgeries
Advantages
- Excellent visibility and access to all cardiac structures
- Ideal for multi-vessel disease or complex anatomy
- Proven long-term outcomes
Limitations
- Larger incision
- Higher postoperative discomfort
- Longer hospital stay
- 6–12 weeks for complete bone healing
- Visible midline scar
What Is Minimally Invasive Cardiac Surgery (MICS)?
Minimally Invasive Cardiac Surgery avoids splitting the breastbone. Instead, surgeons operate through:
- A small incision (4–6 cm) between the ribs
- Right mini-thoracotomy or limited access approach
- Sometimes robotic assistance
- Advanced instruments and imaging guidance
The heart may still be supported with a heart-lung machine, but the surgical trauma is significantly reduced.
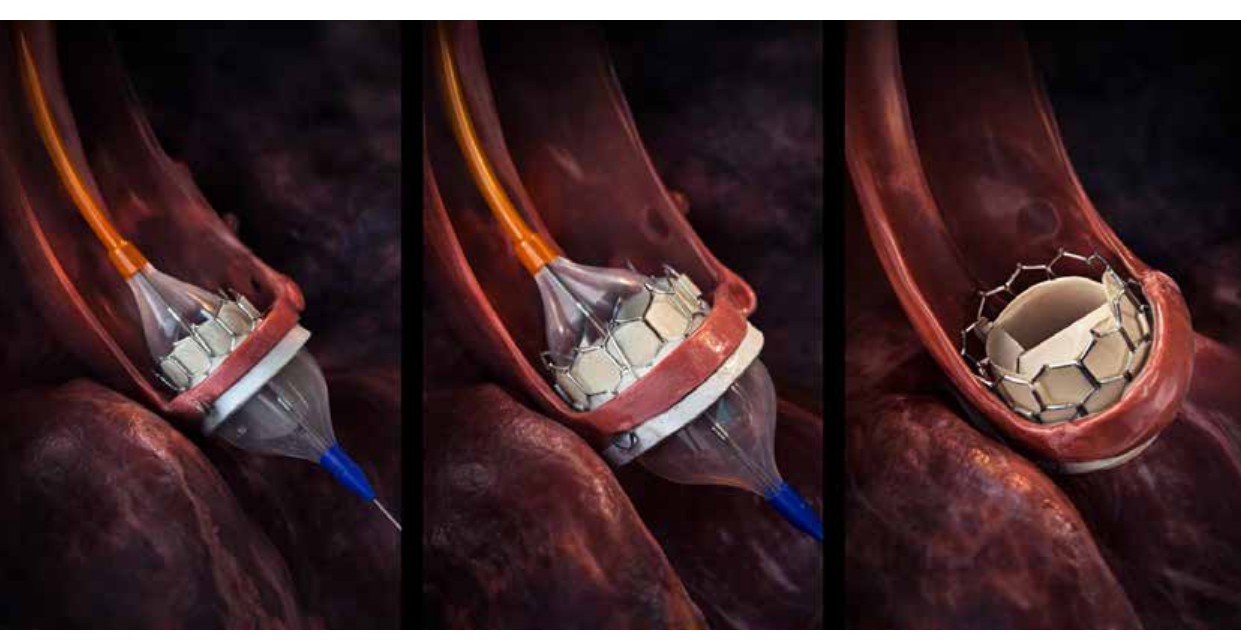
Procedures Commonly Performed Minimally Invasively
- Mitral valve repair
- Aortic valve replacement
- Selected CABG procedures
- Atrial septal defect closure
- Some redo surgeries
Key Differences: MICS vs Traditional Open Surgery
| Feature | Traditional Open-Heart | Minimally Invasive Surgery |
|---|---|---|
| Incision | 8–12 inch midline cut | 4–6 cm side incision |
| Bone Cutting | Sternum divided | No sternotomy |
| Scar | Prominent central scar | Smaller, cosmetically favorable |
| Hospital Stay | 5–10 days | 3–5 days (in selected patients) |
| Recovery Time | 6–12 weeks | 2–4 weeks |
| Post-op Pain | Moderate to high | Significantly less |
| Infection Risk | Slightly higher (sternal wound) | Lower sternal risk |
| Suitability | All complex cases | Selected patients |
Who Is a Candidate for Minimally Invasive Cardiac Surgery?
Not every patient is suitable for MICS. Careful evaluation is essential.
Ideal Candidates
- Isolated valve disease (especially mitral)
- Single-vessel coronary artery disease
- Younger or working professionals needing faster recovery
- Patients concerned about cosmetic outcomes
- Patients without extensive calcification or complex anatomy
Not Suitable If
- Multiple prior chest surgeries
- Severe lung disease
- Complex multi-vessel coronary disease
- Emergency cases
- Extensive aortic disease
A detailed clinical examination, echocardiography, CT imaging, and coronary angiography help determine eligibility.
Benefits of Minimally Invasive Cardiac Surgery
1. Faster Recovery
Patients often return to daily activities within 2–3 weeks.
2. Less Pain
Since the sternum is not divided, postoperative discomfort is significantly reduced.
3. Reduced Blood Loss
Smaller incision often results in fewer transfusions.
4. Lower Infection Risk
No sternal wound reduces the risk of deep chest infection.
5. Better Cosmetic Outcome
Especially important for younger patients and women.
6. Shorter ICU and Hospital Stay
Early mobilization is possible.
When Traditional Open Surgery Is Still the Best Choice
Despite the advantages of minimally invasive techniques, traditional open-heart surgery remains essential in:
- Complex multi-vessel CABG
- Heart transplant surgery
- Mechanical circulatory support implantation (LVAD)
- Combined procedures (valve + bypass)
- Re-operations with dense adhesions
Safety always takes priority over incision size.
Outcomes: Is Minimally Invasive Surgery as Safe?
In experienced hands, minimally invasive cardiac surgery has:
- Comparable success rates
- Similar long-term outcomes
- Reduced hospital complications
- Faster return to normal life
However, outcomes depend heavily on:
- Surgeon expertise
- Institutional infrastructure
- Proper patient selection
Minimally invasive cardiac surgery requires specialized training and advanced surgical skills.
Recovery Timeline Comparison
Traditional Open-Heart Surgery
- ICU stay: 1–3 days
- Hospital stay: 5–10 days
- Resume light activity: 4 weeks
- Complete recovery: 8–12 weeks
Minimally Invasive Cardiac Surgery
- ICU stay: 1 day
- Hospital stay: 3–5 days
- Resume light activity: 1–2 weeks
- Complete recovery: 3–4 weeks
Individual recovery may vary.
Risks Common to Both Approaches
Every heart surgery carries certain risks:
- Bleeding
- Infection
- Stroke
- Arrhythmia
- Kidney dysfunction
- Need for re-intervention
The overall risk depends on:
- Age
- Heart function
- Diabetes
- Kidney status
- Lung health
- Overall medical condition
An experienced cardiothoracic surgeon evaluates these factors carefully before recommending surgery.
Psychological and Lifestyle Impact
Many patients report:
- Greater confidence with smaller scars
- Reduced anxiety about surgery
- Faster emotional recovery
- Earlier return to work
However, surgical success always depends more on quality of repair than incision size.
Making the Right Decision
The choice between minimally invasive and traditional open-heart surgery should never be driven by marketing or cosmetic preference alone.
It must be based on:
- Disease severity
- Anatomical suitability
- Long-term outcomes
- Surgeon expertise
- Patient safety
An experienced cardiothoracic surgeon will guide you toward the safest and most durable solution.
FAQs
1. Is minimally invasive heart surgery completely scar-free?
No. There is still a small incision, but it is significantly smaller and often less visible than traditional surgery.
2. Is it safer than open-heart surgery?
In properly selected patients and experienced centers, it is equally safe.
3. Will I avoid the heart-lung machine?
Not always. Many minimally invasive procedures still use cardiopulmonary bypass.
4. How long does the surgery take?
Minimally invasive procedures may take slightly longer due to technical precision.
5. Is it more expensive?
Costs may vary depending on hospital infrastructure and equipment used.
6. Can elderly patients undergo minimally invasive surgery?
Yes, if they are clinically suitable. Age alone is not a contraindication.
7. What is the most common minimally invasive heart surgery?
Mitral valve repair is among the most commonly performed minimally invasive procedures.
8. Can bypass surgery be done minimally invasively?
In selected single-vessel cases, yes.
9. What about long-term results?
When performed correctly, long-term outcomes are comparable to open-heart surgery.
10. How do I know which option is right for me?
A detailed consultation, imaging evaluation, and risk assessment are essential before making a decision.
About the Doctor
Dr. Asher George Joseph
MBBS, M.Ch (CTVS, Gold Medalist), MRCS (Edinburgh), FACS (USA)
Fellowship in CT Transplantation and Mechanical Circulatory Support (Manchester, UK)
Area of Expertise
- Heart & Lung Transplants
- Advanced Heart Failure Care
- Coronary Artery Bypass (CABG)
- Valve Repairs & Replacements
- Minimally Invasive Heart Surgery
Dr. Asher George Joseph is a highly trained cardiothoracic and vascular surgeon with advanced international training in transplantation and mechanical circulatory support. With a strong academic background and gold medal distinction in CTVS, he specializes in complex cardiac surgeries, advanced heart failure therapies, and minimally invasive cardiac procedures.
For patients requiring precision-driven cardiac care — whether traditional open-heart surgery or minimally invasive approaches — expert evaluation and individualized planning remain the cornerstone of successful outcomes.